Status post tracheostomy is a medical term that refers to a patient who has previously undergone a tracheostomy procedure. This surgical procedure involves creating an opening in the neck to provide an alternative airway for breathing. While tracheostomies are often performed in order to address respiratory or airway complications, their implications go beyond simply allowing the patient to breathe easier. This status indicates that the patient has undergone a significant medical intervention and may require specialized care and attention. Understanding the meaning behind status post tracheostomy can shed light on the challenges and considerations involved in the ongoing care and management of these individuals.
| Characteristics | Values |
|---|---|
| Procedure | Tracheostomy |
| Status | Post |
| Breathing | Through tracheostomy tube |
| Airway | Open |
| Speech | Impaired, may require assistance or alternative communication methods |
| Swallowing | Impaired, may require modified diet or feeding methods |
| Mobility | May be limited due to equipment or tube |
| Care | Requires frequent cleaning and monitoring of tracheostomy site |
| Complications | Risk of infection, blockage, or dislodgement of tracheostomy tube |
| Prognosis | Dependent on underlying condition and reason for tracheostomy |
What You'll Learn
- What is the definition of status post tracheostomy?
- What are the reasons for performing a tracheostomy?
- What are the potential complications or risks associated with a tracheostomy?
- How is the post-operative care for a patient with a tracheostomy different from a patient without one?
- Are there any long-term effects or considerations for individuals who have had a tracheostomy?

What is the definition of status post tracheostomy?
Status post tracheostomy refers to the condition of a patient who has undergone a tracheostomy procedure. A tracheostomy is a surgical procedure that involves creating an opening in the neck to provide an alternative airway for breathing. This procedure is typically performed in cases where a patient is unable to breathe adequately through their nose and mouth due to various reasons such as obstruction, trauma, or respiratory failure.
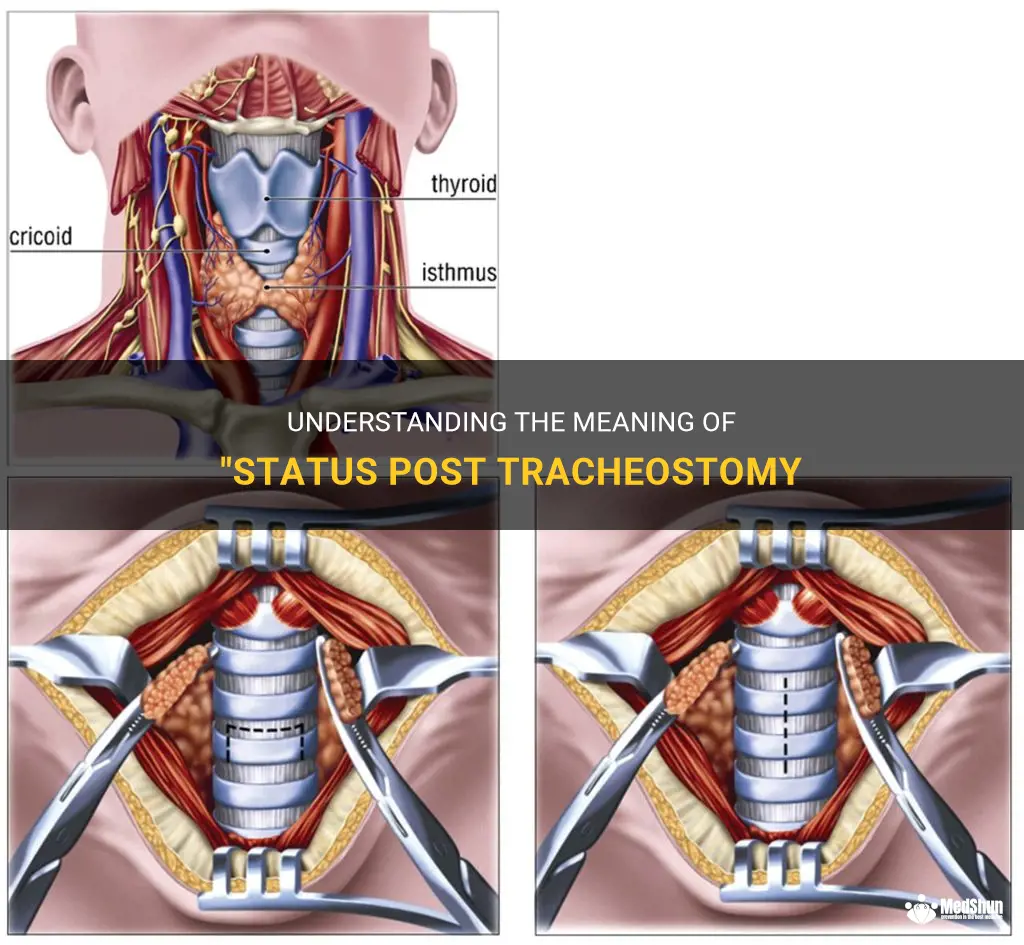
The tracheostomy procedure involves making an incision in the front of the neck and creating a small opening into the trachea, or windpipe. A tracheostomy tube is then inserted through this opening to help maintain an open airway and facilitate breathing. This tube is typically held in place by a secure strap around the patient's neck.
Once a patient undergoes a tracheostomy, they are considered to be in a status post tracheostomy state. This means that the patient has the tracheostomy tube in place and is relying on it for their breathing needs. The patient's condition and progress will be closely monitored by healthcare professionals, as there can be potential complications and ongoing care requirements associated with a tracheostomy.
One of the primary goals of a tracheostomy is to provide a more stable and secure airway. This can be especially beneficial for patients who are at risk of airway collapse, such as those with certain respiratory conditions or those who have experienced trauma to the neck or chest. By creating a direct opening into the trachea, the tracheostomy tube bypasses any obstructions or restrictions in the upper airway, allowing for easier and more efficient breathing.
In addition to providing a secure airway, a tracheostomy can also facilitate other aspects of patient care. For example, it can enable easier suctioning of secretions from the airway, reduce the risk of aspiration pneumonia, and provide a route for delivery of certain medications or oxygen.
However, while a tracheostomy can be a life-saving procedure, it is not without its risks and complications. Some potential complications of a tracheostomy include infection, bleeding, damage to surrounding structures, tube displacement or obstruction, and difficulty speaking or swallowing. Close monitoring and care are essential to minimize these risks and ensure the patient's safety and well-being.
The management of a patient in a status post tracheostomy state involves regular assessment of the tracheostomy site and the surrounding tissue for signs of infection or other complications. The tracheostomy tube may need to be cleaned and replaced periodically to prevent blockages and infections. Suctioning of the airway may also be required to remove secretions and maintain proper airflow.
Additionally, healthcare professionals will educate and train patients and their caregivers on how to care for the tracheostomy tube and how to manage any potential complications or emergencies. This may include teaching proper technique for tube cleaning and changing, recognizing signs of infection or blockage, and knowing how to perform emergency procedures such as cuff deflation or decannulation.
In conclusion, status post tracheostomy refers to a patient who has undergone a tracheostomy procedure. This surgical procedure involves creating an opening in the neck to provide an alternative airway for breathing. Patients in a status post tracheostomy state require ongoing care and monitoring to ensure the proper function and maintenance of the tracheostomy tube. Understanding the risks, complications, and necessary care associated with a tracheostomy is crucial for healthcare professionals and caregivers involved in the management of these patients.
The Importance of Regular Tracheostomy Suctioning: Ensuring Proper Airway Hygiene and Functionality
You may want to see also

What are the reasons for performing a tracheostomy?
A tracheostomy is a surgical procedure that involves creating an opening in the front of the neck and into the trachea (windpipe). This opening, known as a stoma, allows direct access to the trachea and is used for various medical reasons. Here, we will discuss the reasons why a tracheostomy may be performed.
- Airway Obstruction: Tracheostomy may be necessary in cases where there is a partial or complete blockage of the upper airway. This can occur due to tumors, swelling, trauma, or foreign bodies. A tracheostomy provides a bypass for the blocked airway and allows for normal breathing.
- Respiratory Failure: In some cases, a tracheostomy is performed to manage respiratory failure. This can occur in conditions such as chronic obstructive pulmonary disease (COPD), respiratory muscle weakness, or severe pneumonia. By directly accessing the trachea, a tracheostomy tube can be connected to a ventilator or other respiratory support devices to assist with breathing.
- Long-term Mechanical Ventilation: Some patients require long-term mechanical ventilation due to chronic conditions that prevent them from breathing adequately on their own. A tracheostomy allows for the placement of a breathing tube directly into the trachea, eliminating the need for an endotracheal tube that is typically used during short-term ventilation.
- Head and Neck Surgery: Tracheostomy may be performed as a part of head and neck surgery. This can be necessary to maintain a clear airway during surgery or postoperatively if there is a risk of airway compromise due to tissue swelling or bleeding.
- Airway Protection: Tracheostomy can be used in patients who are at risk of aspirating (inhaling) their own secretions or liquids into their lungs. By accessing the trachea, a suction catheter can be inserted into the tracheostomy tube to remove secretions and prevent respiratory complications.
- Weaning from Ventilator: Some patients who have been on a mechanical ventilator for a long time may require gradual weaning to improve their ability to breathe on their own. A tracheostomy allows for easier weaning by providing access for gradual reduction in ventilatory support.
- Neurological Disorders: Tracheostomy may be performed in individuals with severe neurological disorders such as spinal cord injuries, amyotrophic lateral sclerosis (ALS), or brainstem lesions. These conditions can cause respiratory muscle weakness or paralysis, and a tracheostomy can assist with breathing in these patients.
It is important to note that the decision to perform a tracheostomy is made on an individual basis after a thorough evaluation of the patient's clinical condition, prognosis, and anticipated benefits. The procedure is typically performed by a surgeon experienced in airway management and requires careful monitoring and follow-up care to prevent complications and promote healing.
In conclusion, tracheostomy is performed for various reasons, including airway obstruction, respiratory failure, long-term ventilation, head and neck surgery, airway protection, weaning from a ventilator, and neurological disorders. The procedure provides direct access to the trachea and can significantly improve the patient's respiratory function and quality of life.
Tips and Techniques for Weaning from Tracheostomy to Trach Collar
You may want to see also

What are the potential complications or risks associated with a tracheostomy?
A tracheostomy is a surgical procedure that creates an opening in the front of the neck to access the airway. It is usually performed in cases where there is an obstruction in the upper airway or when a patient requires long-term mechanical ventilation. While a tracheostomy can be life-saving, it also carries certain risks and potential complications.
One of the most immediate risks of a tracheostomy is bleeding. During the surgery, blood vessels in the neck may be damaged, leading to bleeding. Although this is typically controlled during the procedure, there is always a risk of postoperative bleeding. This can be a serious complication and may require immediate intervention to stop the bleeding.
Infection is another potential complication of a tracheostomy. The opening in the neck creates a direct pathway for bacteria to enter the airway and cause an infection. To reduce the risk of infection, the tracheostomy site needs to be cleaned and maintained with proper care. Antibiotics may also be prescribed to prevent or treat any infection that may occur.
Some patients may develop granulation tissue around the tracheostomy site, which can cause blockage or make it difficult to insert the tracheostomy tube. Granulation tissue is the body's natural response to injury, and it can form in the healing process after a tracheostomy. If granulation tissue becomes problematic, it may require removal or treatment to prevent complications.
The tracheostomy tube itself can cause complications. One of the most common issues is accidental decannulation, where the tube becomes dislodged or removed. This can lead to breathing difficulties and may require emergency intervention to re-establish the airway. It is important for caregivers and healthcare professionals to be vigilant and ensure the tracheostomy tube remains securely in place.
Another potential risk is damage to surrounding structures during the surgery. The trachea, esophagus, blood vessels, and nerves are all in close proximity to the trachea. If these structures are inadvertently injured during the procedure, it can result in serious complications such as airway compromise, vocal cord paralysis, or damage to blood vessels.
One of the long-term complications of a tracheostomy is the formation of a tracheal stenosis. This occurs when scar tissue forms and narrows the trachea, making it difficult for air to flow freely. Tracheal stenosis may cause breathing difficulties and require additional interventions, such as balloon dilation or surgical repair.
Lastly, prolonged use of a tracheostomy tube can lead to complications such as pressure ulcers or damage to the tracheal mucosa. Proper care and maintenance of the tracheostomy tube can help prevent these complications. Regular cleaning, monitoring the skin around the tracheostomy site, and using appropriate dressings can reduce the risk of pressure ulcers or irritation to the skin.
In conclusion, while a tracheostomy can be life-saving in certain situations, it is not without risks. Complications such as bleeding, infection, granulation tissue formation, accidental decannulation, damage to surrounding structures, tracheal stenosis, pressure ulcers, and mucosal damage can occur. It is important for healthcare professionals and caregivers to be aware of these potential risks and take appropriate measures to prevent and manage complications. Regular monitoring and proper care of the tracheostomy site are essential to minimize the likelihood of complications and ensure the best possible outcome for the patient.
Exploring the Wide Array of Tracheostomy Tube Varieties
You may want to see also

How is the post-operative care for a patient with a tracheostomy different from a patient without one?
After undergoing a tracheostomy, it is important for patients to receive specialized post-operative care. A tracheostomy is a surgical procedure that creates an opening in the neck leading to the trachea, which allows for the insertion of a breathing tube. This procedure is often performed to assist with breathing for patients who are unable to breathe spontaneously or effectively on their own.
One of the main differences in post-operative care for a patient with a tracheostomy compared to a patient without one is the need for ongoing maintenance and care of the tracheostomy tube. This includes regular cleaning and suctioning of the tube to prevent blockages and ensure proper airflow. The tracheostomy site must also be kept clean and dry to reduce the risk of infection.
Another important aspect of post-operative care for tracheostomy patients is monitoring and managing secretions. Due to the presence of the tracheostomy tube, patients may have increased mucus production, which can lead to coughing or difficulty breathing. Regular suctioning is necessary to remove excess secretions and maintain a clear airway.
In addition, tracheostomy patients may require a special diet or modified feeding techniques. The presence of the tracheostomy tube can interfere with swallowing and increase the risk of aspiration. Some patients may need to be fed through a feeding tube to ensure proper nutrition while minimizing the risk of complications.
Furthermore, tracheostomy patients may require additional respiratory support and monitoring compared to patients without a tracheostomy. This can include the use of supplemental oxygen, humidification of the inspired air, and regular monitoring of oxygen saturation levels.
It is also important to provide adequate patient education and support to tracheostomy patients and their caregivers. This includes instruction on proper tracheostomy care, recognizing signs of infection or complications, and emergency management techniques. Patients and caregivers should also be educated on the importance of regular follow-up visits and adherence to medical appointments.
Overall, the post-operative care for a patient with a tracheostomy is more complex and requires specialized knowledge and skills. Ongoing monitoring, maintenance of the tracheostomy tube, management of secretions, dietary modifications, additional respiratory support, patient education, and caregiver support are all essential components of post-operative care for these patients. By providing comprehensive care, healthcare providers can help ensure the best possible outcomes for tracheostomy patients and improve their overall quality of life.
Understanding the Causes of Tracheostomy in Babies: A Comprehensive Guide
You may want to see also

Are there any long-term effects or considerations for individuals who have had a tracheostomy?
A tracheostomy is a surgical procedure that creates an opening in the front of the neck and directly into the windpipe (trachea). This opening, called a tracheostomy or stoma, allows for breathing when the usual route for breathing is obstructed or compromised.
While tracheostomies are often performed as a temporary measure to assist with breathing during a medical emergency or illness, some individuals may require a tracheostomy as a long-term or permanent solution. In such cases, it is important to understand the potential long-term effects and considerations associated with this procedure.
One of the main long-term effects of having a tracheostomy is the impact on speech and communication. As the tracheostomy bypasses the vocal cords, it can limit the individual's ability to produce sound. However, with proper speech therapy and the use of specialized devices such as speaking valves, many individuals with tracheostomies can regain some level of speech and communication.
Another long-term consideration is the need for ongoing care and maintenance of the tracheostomy site. Regular cleaning, changing of dressings, and suctioning may be required to prevent infection and ensure proper airflow. It is important for individuals with tracheostomies and their caregivers to receive training and education on tracheostomy care and to have access to appropriate medical supplies.
Additionally, having a tracheostomy can affect the individual's ability to perform certain activities. Swimming, for example, may require additional precautions to prevent water from entering the tracheostomy site. It is crucial for individuals with tracheostomies to discuss any limitations or concerns with their healthcare team to ensure they can safely participate in activities they enjoy.
Psychosocial implications should also be taken into account. Having a visible tracheostomy tube can affect an individual's self-esteem and overall well-being. It is important for individuals with tracheostomies to have access to emotional support, counseling, and resources to address any psychological or emotional challenges they may face.
Finally, it is essential to have a plan in place for emergencies and unforeseen events. Individuals with tracheostomies should have a backup tracheostomy tube, emergency contact information easily accessible, and knowledge of what to do in case of tube dislodgement or blockage.
In conclusion, individuals who have had a tracheostomy may experience various long-term effects and considerations. These can include limitations in speech and communication, the need for ongoing care and maintenance, impact on activities, psychosocial implications, and the importance of emergency preparedness. It is crucial for individuals with tracheostomies to work closely with their healthcare team to ensure proper care, support, and education to optimize their quality of life.
How to Conceal a Tracheostomy: Tips and Techniques for Discretion
You may want to see also
Frequently asked questions
"Status post tracheostomy" refers to the current condition of a patient who has undergone a tracheostomy procedure in the past. This means that the patient has had a surgical incision made in their neck to create an opening into the trachea, or windpipe, to help with breathing.
A tracheostomy may be necessary for various medical reasons. It is often performed when a person has difficulty breathing due to an obstruction in their upper airway, or when they are unable to breathe on their own due to a medical condition or injury. It can also be used to assist with long-term ventilation or to help remove secretions from the airway.
While tracheostomies are generally safe procedures, they do come with some potential risks and complications. These can include infection at the surgical site, bleeding, scarring, damage to nearby structures (such as blood vessels or vocal cords), and difficulties with speaking or swallowing. It is important for patients with a tracheostomy to receive proper care and monitoring to prevent and manage these complications.
After a tracheostomy, the patient will need ongoing care and management. This involves regular cleaning and changing of the tracheostomy tube, monitoring for any signs of infection or complications, and ensuring proper humidification and moisture for the airway. Patients may also require assistance with tracheostomy care from healthcare professionals or trained caregivers.
In some cases, a tracheostomy can be temporary and eventually be closed or reversed. This depends on the underlying condition that necessitated the tracheostomy and the progress of the patient's recovery. Reversal of a tracheostomy typically involves a surgical procedure to close the tracheostomy site and restore normal breathing through the mouth and nose. The decision to reverse a tracheostomy is made by the healthcare team in collaboration with the patient based on their individual needs and medical condition.